Manhattan Physical Therapy
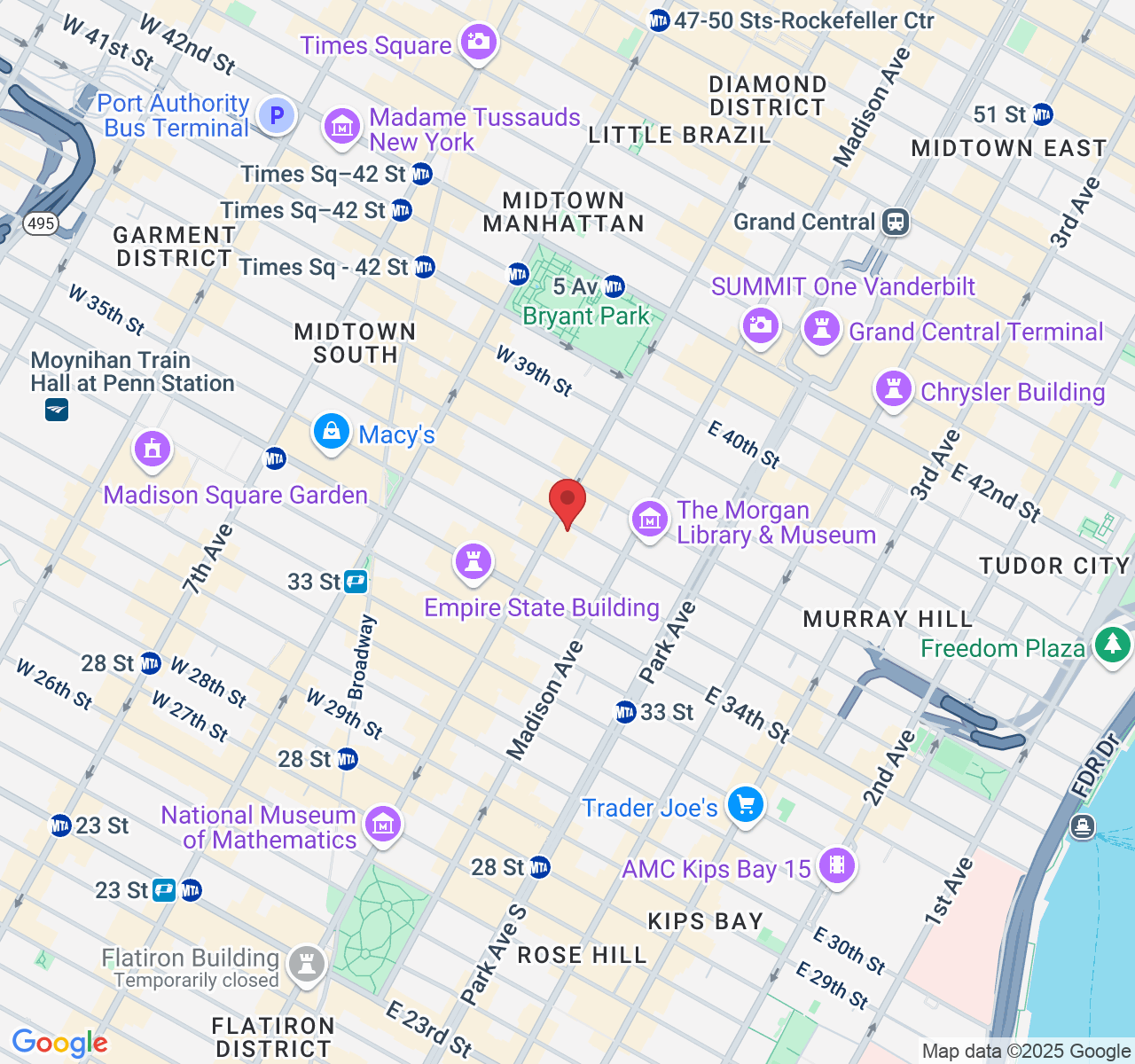
Physical Therapy & Acupuncture located in New York, NY
Manhattan Physical Therapy
PHYSICAL THERAPY & ACUPUNCTURE LOCATED IN NEW YORK, NY

About Manhattan Physical Therapy
Manhattan Physical Therapy is a leading pain relief and injury ...

About Manhattan Physical Therapy
Manhattan Physical Therapy is a leading pain relief and injury ...
Services
Suspension Therapy
Bell's Palsy
Acupuncture
Sports Performance
3D Movement Scan
Diagnostics Ultrasound
Pelvic Floor
Pain Management
Services
Suspension Therapy
Bell's Palsy
Acupuncture
Sports Performance
3D Movement Scan
Diagnostics Ultrasound
Pelvic Floor
Pain Management
Meet The Doctors

Tiffany Zarcone, PT, DPT
John Miller

Bianca Guidotti, AT
Meet The Doctors

Tiffany Zarcone, PT, DPT
John Miller

Bianca Guidotti, AT
Our Mission
Manhattan Physical Therapy and Pain Center is a leader in pain relief and injury recovery located in Midtown New York City. The four specialized physical therapists on staff go beyond standard physical therapy by challenging their clients' bodies to build core strength, flexibility, and increase range of motion.
Manhattan Physical Therapy and Pain Center has an excellent track record of success treating back pain caused by strains, degenerative disc disease, piriformis syndrome, spondylolisthesis or whiplash injuries.
Our Mission
Manhattan Physical Therapy and Pain Center is a leader in pain relief and injury recovery located in Midtown New York City. The four specialized physical therapists on staff go beyond standard physical therapy by challenging their clients' bodies to build core strength, flexibility, and increase range of motion.
Manhattan Physical Therapy and Pain Center has an excellent track record of success treating back pain caused by strains, degenerative disc disease, piriformis syndrome, spondylolisthesis or whiplash injuries.
Insurances
We accept most insurance providers. If you have specific questions regarding your coverage, please contact us for additional information.








Insurances
We accept most insurance providers. If you have specific questions regarding your coverage, please contact us for additional information.








Manhattan Physical Therapy
✆ Phone (appointments):
(212) 213-3480
Address: 385 5th Ave, Suite 503, New York, NY 10016